Project Summary
Key risk factors for ambulatory sensitive hospitalisation (ASH) include inadequate vaccination, lack of early detection and treatment of acute conditions, and inadequate control of chronic conditions. Social determinants affect health, and inequalities exist by population groups; there is some evidence that rates for males are higher, as are those for Māori and Pacific children and those who live in more deprived areas. Universal mass vaccination programmes are an effective preventive measure, and evidence for the effectiveness of community water fluoridation is strong.
For New Zealand children, ASHs account for approximately 30% of all acute and arranged medical and surgical discharges each year. The leading causes include respiratory, dental, dermatological and gastroenteritis ASH conditions. Evidence shows that rates differ by age, gender, ethnicity and area-level deprivation. It is now recognised that ASH rates may also be influenced not only by primary care, but by broader policy measures or social determinants. In addition to exploring variation by key demographic factors such as age group, ethnicity and area-level deprivation, more research is needed that investigates spatial variation and other wider influences of childhood ASH rates, such as community water fluoridation, vaccination or enrolment in health services. For the purpose of this report under 5 refers to 0–4 years of age and under 13 refers to 5–12 years.
A wide range of factors affect ASH rates in primary health organisations (PHO):
• ASH rates vary by age, ethnicity, area-level deprivation, and rural/urban classification.
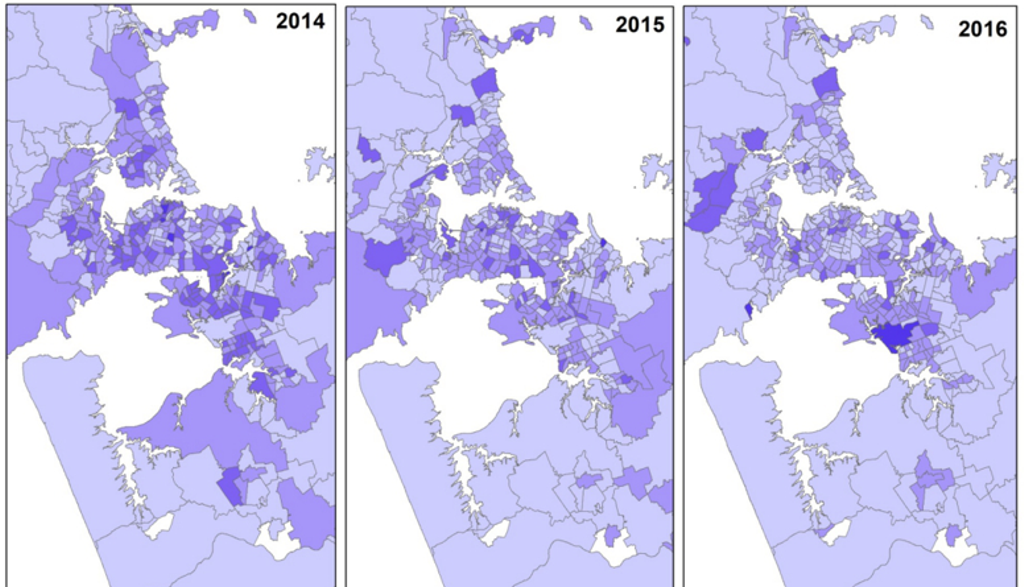
• Spatial variation in ASH rates by district health board was present.
• The highest ASH rate was generally in areas with health service availability of up to 30 minutes’ driving time.
• Areas with fluoridated water were associated with lower dental ASH rates, and there was some evidence that this difference was exaggerated in the most deprived areas.
• Gastroenteritis ASH rates declined following the introduction of the rotavirus vaccine.
• A higher percentage of enrolment in PHOs was related to lower ASH rates.
This report uses several nationwide cross-sectional surveys and registries to add novel findings to current evidence regarding ASH rates within New Zealand. It identifies spatial variation in both health service availability and ASH rates by age group (under 5 and under 13 years) and demonstrates evidence that ASH rates were also affected by wider factors such as water fluoridation, vaccination and enrolment in PHOs. There was also notable variation by area-level deprivation and ethnicity. All limitations are fully outlined in a longer report that can be requested by emailing GeoHealthLab@canterbury.ac.nz